Manuscript accepted on : 17-03-2022
Published online on: 31-05-2022
Plagiarism Check: Yes
Reviewed by: Dr. Feng Xue
Second Review by: Dr. Hind Shakir , Dr. Ana Golez
, Dr. Ana Golez
Final Approval by: Dr. Eugene A. Silow
Heart Rhythms Recorded Among Pupils in Enugu, South East Nigeria
Pamela Onyinye Okorie1 , Princewill Ikechukwu Ugwu1*
, Princewill Ikechukwu Ugwu1* , Godsent Chichebem Isiguzo2
, Godsent Chichebem Isiguzo2 , Okechukwu Maduabuchi Omire-Oluedo1
, Okechukwu Maduabuchi Omire-Oluedo1 , Choice Chinemerem Nworgu1
, Choice Chinemerem Nworgu1 , Vivian Ifeyinwa Nwannadi1
, Vivian Ifeyinwa Nwannadi1 , Oluchi Kizito Okafor1
, Oluchi Kizito Okafor1 , Ugochukwu Bond Anyaehie1
, Ugochukwu Bond Anyaehie1
1Department of Physiology, Faculty of Basic Medical Sciences, College of Medicine, University of Nigeria, Enugu Campus, Enugu, Nigeria.
2Department of Medicine, Federal Medical Centre, Abakiliki, Ebonyi, Nigera.
Corresponding Author E-mail: princewill.ugwu@unn.edu.ng
DOI : http://dx.doi.org/10.13005/bbra/2998
ABSTRACT:
Electrocardiography (ECG) is an important non-invasive tool used to detect cardiac arrhythmias. Abnormal, and indeed dangerous, rhythms may exist among apparently healthy school children. Regular cardiovascular screening may help reveal such abnormal rhythms and thus help to prevent unexpected adverse events, including sudden death. The aim of this study was to ascertain the different heart rhythms that occur in pupils in Enugu metropolis. A descriptive cross-sectional research approach was adopted. Three hundred and fourty-one healthy looking pupils between age six and twelve years were recruited. Questionnaires were administered; medical general examination and electrocardiography, using a 12-lead ECG machine, were done on each of the pupils. At the end of the study, no structural evidence of heart disease was identified in any of the pupils. There was normal sinus rhythm in 79.1% of the pupils, however, in 20.9% of them abnormal rhythm was seen. The abnormal rhythms noted were: premature complexes (8.44%), atrial tachycardia (5.64%), first degree atrioventricular block (5.63%), bradycardia (2.82%) and incomplete right bundle block (2.82%). This study showed that among apparently healthy school children, abnormal heart rhythms are present, and these rhythms could be missed in absence of cardiovascular screening. As the reported cases of sudden death during sports in children and young adults keep rising, it is important to encourage routine cardiovascular screening to aid early detection and prevention of possible abnormalities.
KEYWORDS: Apparently Healthy; Abnormal; Electrocardiography; Heart rhythm; Pupils
Download this article as:| Copy the following to cite this article: Okorie P. O, Ugwu P. I, Isiguzo G. C, Omire-Oluedo O. M, Nworgu C. C, Nwannadi V. I, Okafor O. K, Anyaehie U. B. Heart Rhythms Recorded Among Pupils in Enugu, South East Nigeria. Biosci Biotech Res Asia 2022;19(2). |
| Copy the following to cite this URL: Okorie P. O, Ugwu P. I, Isiguzo G. C, Omire-Oluedo O. M, Nworgu C. C, Nwannadi V. I, Okafor O. K, Anyaehie U. B. Heart Rhythms Recorded Among Pupils in Enugu, South East Nigeria. Biosci Biotech Res Asia 2022;19(2). Available from: https://bit.ly/3N4HFhw |
Introduction
The relationship between sudden death and cardiovascular abnormalities continues to receive increasing attention, especially with the rise in incidence of sudden death in young peopleglobally.1Cardiovascular diseases like Ischaemic Heart disease and cardiovascular accidents are among the leading causes of death worldwide. There is increasing advocacy for routine medical, especially cardiovascular system, checks for young individuals participating in sporting activity. Not much of such advocacy is being pushed in sub-Saharan Africa, and indeed in Nigeria, for pupils and students in schools despite the physical exertion they undertake daily.1
Electrocardiography (ECG) is an important non-invasive test used to monitor and interpret cardiac rhythms. The ECG can detect cardiac arrhythmias, myocardial infarctions and other cardiac electrical conducting system abnormalities.2The standard 12-lead ECG is the most commonly used ECG variety.
Heart arrhythmias are quite common as they occur in many individuals around the world. A large number of these rhythm changes are benign. Dangerous rhythm abnormalities may exist among apparently healthy school children and regular cardiovascular screening may help reveal such and thus prevent unexpected adverse events, including sudden death.1,2 There is dearth of studies done on the ECG readings of pupils, aged 6 to 12 years old, in South-Eastern Nigeria. Hence this study sought to identify the common heart rhythms among school pupils in Enugu, south east Nigeria.
Materials and Methods
In this study, a descriptive cross-sectional study approach was adopted. The study was done in Enugu, the ancient capital city of Enugu State, between October 2018 and May 2019. A sample size of three hundred and ten (310) was calculated. However, using a method previously described in literature, a total of three hundred and forty-one (341) apparently healthy children were recruited.3
Inclusion criteria involved apparently healthy asymptomatic children aged 6 to 12 years. Children with diagnosed morbidities such as: sickle cell disease, HIV/AIDS, lung diseases, congenital or acquired heart diseases, evidence of pallor or jaundice on examination were excluded from the study. Interviewer-administered questionnaires were used to obtain information from parents of the recruited children. Information obtained included personal bio data, social family history (the part of the metropolis they lived in, the setting they lived in; how many of them lived in a room), past medical history (suggestive of any chronic illness), symptoms of cardiac disease if any, and drug history (use of antiretroviral drugs, anti-arrhythmic drugs, drugs for management of sickle cell anemia).
Ethical Approval
The ethical approval for the work was obtained from the Research and Ethics committee of the College of Medicine, University of Nigeria Enugu Campus, Enugu, Enugu State, with protocol number 052/09/2018.
Informed Consent
Parents of all the children who participated in this study gave written informed. consent was also obtained from the older children. The data collected was stored, and confidentiality was ascertained.
Physical examination was done on each of the participants. The body mass index (BMI) was calculated for each child as the weight in kilograms (kg) divided by a square of the height in meters (m). The height of each participant was measured using a stadiometer; while the weight was measured with a weighing balance. The blood pressure was measured in both arms with patient sitting using a mercury sphygmomanometer (Bokang, Germany) and stethoscope (Littmann model, China).4 An appropriately sized cuff was placed on the arm with the cuff covering at least eighty percent of the arm. Simultaneously, systolic blood pressure was estimated by palpated radial pulse obliteration pressure and the cuff was then inflated 10–20 mmHg above the level obtained by palpation for the auscultatory determinations. Once two or more initial sounds (Korotkoff sounds) were heard, that point was taken as the systolic blood pressure; and the point of eventual cessation of Korotkoff sounds was taken as the diastolic blood pressure.
The children were called in batches into the examination room provided by the school and church authorities after 10- 12 hours of overnight rest. A demonstration of the ECG procedure was done for the children to observe. Taking turns, each child had a standard 12-lead ECG recording, using a portable digital electrocardiograph, as specified by the American Heart Association.5 The 12-lead ECG tracing was recorded using a 210mm tracing paper at a speed 25m/s and frequency H50 d 55 Hz. A minimum of five cardiac cycles were recorded per ECG lead; measuring along the vertical line of the ECG graph paper, 10 mm represented 1 mV, whilst 1mm along the horizontal line represented 0.04s(40ms).
To improve the quality of the ECG recording, the skin over the chest wall and limbs of each child was cleaned before procedure.6-8 Arrow ECG electrode jelly was used to provide effective contact between the skin and electrode. Cotton wool and methylated spirit were used to clean the skin before the gel was applied. Electrodes were placed on the arms and legs distal to the shoulders and hips, and thus not necessarily on the wrists and ankles.9,10 Six electrodes were placed on the chest in the following locations: the V1 electrode was placed in the fourth intercostal space at the right sternal border; the V2 electrode was positioned in the fourth intercostal space at the left sternal border; the V3 electrode was placed midway between V2 and V4 electrodes; the V4 electrode was placed in the fifth intercostal space in the mid-clavicular line; the V5 electrode was positioned in the horizontal plane of V4 at the anterior axillary line; and the V6 electrode was placed in the horizontal plane of V4 at the mid-axillary line.
Statistical Package for Social Sciences (SPSS) version 20 was used to analyse the data obtained from the study. The student t-test was used for comparing the means, while binary logit regression was used for determination of predicting factors of ECG abnormalities. Values of p < 0.5 were taken as statistically significant.
Results and Discussion
This study assessed the heart rhythms of pupils, aged between 6 and 12 years, in a selected location in Enugu, Nigeria. 157(46%) male and 184(54%) female 6-12 year-old kids formed the participants of this work. The average age of the children was 9.2(± 1.6) years; their mean weight and height were 34.5(8.9) kilograms and 1.4 (±0.1) meters respectively. Those that have undergone disease screening of any type, including electrocardiography, were 132(38.7%); while those that have not undergone screening of any type in the past were 209 (61.3%). Mean diastolic blood pressure and mean systolic blood pressure were 59 (±10.7) mmHg and 90.8 (±10.6) mmHg respectively (Table 1). None of the children had structural evidence of heart disease, and throughout the duration of the study, no abnormal events occurred. Comparing the BMI, age, systolic and diastolic blood pressures of children with normal and abnormal ECG findings, BMI and age showed significant correlation, with p values 0.041* and 0.001* respectively (Table 2). The prevalence of normal sinus rhythm was 79.1%, while abnormal rhythm was seen in 20.9% of the participants (Figure 1). During the study, the following abnormal rhythms were recorded: premature complexes (8.44%); atrial tachycardia (5.64%); first degree atrioventricular block(5.63%); bradycardia (2.82%) and incomplete right bundle block 2.82% (Figure 2).
In 0.2–2.2% of normal children, isolated ventricular premature beatings may be seen on a routine resting ECG.11 However, in this current study, premature complex rhythms accounted for 8.44% of the ECG abnormalities identified. In a particular report, premature beats found in 14% of the infants studied were supraventricular beats.12 Supraventricular premature beats have been reported in between 15– 40% of older children in a study. Hence, there appears to be an age related variation in occurrence of PVCs in apparently healthy children. About twenty percent of newborns have uncomplicated ventricular ectopic beats consisting of uniform PVCs or couplets.13 Uncomplicated ventricular ectopic beats is seen in 10% of toddlers and school-age children and increases to between 20% to 30% in normal adolescents.14-17 Although having some ventricular ectopic beats is common in otherwise normal adolescent boys, multiform PVCs, couplets, or non-sustained VT can be seen in less than 2% of them during 24-hour monitoring, and less than 5% will have more than 50 beats per 24 hours.14,15,18
Premature ventricular contractions (PVC) have been reported to be more common in older folks, especially elderly men, but can occur at any age even in a healthy person.19 PVCs have been reported to occur spontaneously, with no known cause, in a very significant proportion of people, and may be indicative of a hidden cardiac pathology. So, finding PVCs requires a more elaborate cardiac check. High blood calcium, cardiomyopathy – hypertrophic or dilated, hypoxia, mitral valve prolapse, magnesium and potassium deficiency, lack of sleep/exhaustion and stress have all been fingered as possible causatives of PVCs. 19, 20
Investigating PVCs usually would involve thorough history taking and physical examination, electrocardiography, echocardiography and Holter monitoring.21, 22, 23
The major problem faced in most developing and underdeveloped countries in the world is lack of screening culture probably due to ignorance and poverty, thus PVCs may not be identified on time and followed up appropriately to avoid the incidence of sudden death among various age groups.
Atrial tachycardia (AT) accounted for 5.64% of the abnormalities. Atrial tachycardia has been noted to occur in children with otherwise normal hearts but it can occur along with other congenital heart problems.24-26 Basically, AT is seen as a type of supraventricular tachycardia (SVT). In AT, heart rate can range between 100 to 300 beats per minute .24-26 AT can easily be found in children who have congenital cardiac abnormalities, but its occurrence is not limited to this age group. Another less common cause of supraventricular tachycardia in kids is Focal atrial tachycardia (FAT). FAT occurs because of the presence of abnormal and exaggerated discharge from a non-sinus origin in the atrium.27-29 FAT usually manifests as continuous arrhythmias. FAT will usually easily lead to tachycardia-induced cardiomyopathy, preventable by prompt control of the arrhythmia.30-32 Ectopic atrial tachycardia (EAT) is a frequent reason for manifestation of persistent supraventricular tachycardia in the young (prevalence of 0.34% to 0.46%).33-35 The life history of ectopic atrial tachycardia includes possible progression to congestive cardiac failure and it features as a reversible cause of cardiomyopathy.33-37 EAT and permanent junctional reciprocating tachycardia constitute a minor proportion of SVTs, but they are a major cause of Tachycardia Induced Cardiomyopathy (TIC) seem in infants and children less than 5 years old.38 The cardiomyopathy results from the erratic nature of these tachycardias in most of the patients.35,37,38,39 Typically in ectopic atrial tachycardia we find a continuous atrial tachycardia and an irregularly heart rate which is too fast for the child’s age.36,40,41 Possible causes of atrial tachycardia include a problematic heart valve and weak or inflamed heart muscles/tissue.42
When the PR interval is more than 200 millisecond on an electrocardiogram (ECG), a first-degree atrioventricular block is said to have occurred. Such heart blocks are known not to show any symptoms typically and usually have no significant complications, as they are only spotted through an ECG reading. Basically treatment is not required in first-degree heart blocks. In such cases routine observation is done to ensure the condition is not worsening, in which case there would be increased conduction delay.43,44 First degree heart block accounted for 5.63% of the abnormalities in this study. Previous studies have shown that prevalence of first degree heart block in apparently healthy individuals increases with age, and can rise to as high as approximately 6.0% by age of 60 years. Male folks are two times more affected than females. In particular, about 10% of active athletes have been reported to have first degree heart block features. This finding in young athletes suggests that rigorous exercise-induced parasympathetic autonomic firings may play causative a role in etiology of first-degree AV block in these atheletes.45, 46
First or second degree block can be seen in children with congenital heart defects, diphtheria, rheumatic carditis and patients having digoxin overdose.47 Though generally considered as benign, first-degree heart blocks may be associated with atrial arrhythmias which may need pacemaker implantation to prevent mortality.48
Abnormal sinus bradycardia is not commonly seen in children. It appears most times following cardiac surgery. It could be due to increase vagal tone and inherited arrhythmias.49 Conduction delay or incomplete right bundle branch block constituted 2.82 % of the abnormalities reported. Data on prevalence of Right Bundle Branch Block (RBBB) in less than 12-year-old population is limited. In one study, 2.94% of 20,000 apparently healthy children had incomplete RBBB, while 0.16% had complete RBBB.50 This could probably due to conduction system disease in some individuals.51
Previous studies have shown that ECG could be influenced by age, sex, nutrition and race.52-55 In this study, the BMI of the children was within normal limits. So, we could not possibly draw a correlation of BMI with ECG abnormalities noted. A larger population study may provide more evidence, however a study postulated that obesity does not result in pathologic ECG phenomena in children.56
We report age as a possible predictor of ECG abnormalities, similar to previous studies by Hiss et al.57 This could probably be explained that as age increases there is decrease in sympathetic activity, increase in parasympathetic activities and age-related desensitization/degeneration of the sinus node.58, 21
Table 1: Socio -demographics of the children aged 6-12 years
| Variables | Frequency | Percentage | Mean (SD) |
| Sex
Male Female Total |
157 184 341 |
46.0 54.0 100.0 |
|
| Age (Years)
6 to 9 10 to 12 Total |
172 169 341 |
50.4 49.6 100.0 |
9.2±1.6 |
| Screening in the past
Yes No Total |
132 209 341 |
38.7 61.3 100.0 |
|
| Weight(kilogram) | 341 | 100.0 | 34.5 ±8.9 |
| Height(meters) | 341 | 100.0 | 1.4 ±0.1 |
| BMI | 341 | 100.0 | 17.2 ±2.8 |
| Systolic BP(mmHg) | 341 | 100.0 | 90.8 ±10.6 |
| Diastolic BP(mmHg) | 341 | 100.0 |
59 ±10.7 |
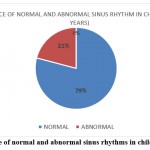 |
Figure 1: Prevalence of normal and abnormal sinus rhythms in children aged 6-12years. |
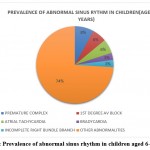 |
Figure 2: Prevalence of abnormal sinus rhythm in children aged 6-12 years. |
Table 2: Comparing BMI, Blood pressure and age of children with normal and abnormal ECG findings.
| Parameter | ECG Status | Mean±SD |
| BMI | Normal | 17.49±2.99 |
| Abnormal | 16.88±2.35 | |
| SBP | Normal | 91.40±10.37 |
| Abnormal | 89.98±10.87 | |
| DBP | Normal | 60.27±7.92 |
| Abnormal | 58.89±8.02 | |
| Age | Normal | 8.83±1.69 |
| Abnormal | 9.43±1.51 |
Conclusion
In conclusion, this study showed that among apparently healthy school children, abnormal heart rhythms are present, and these rhythms could be missed in absence of cardiovascular screening. As the reported cases of sudden death during sports in children and young adults keep rising, it is important to encourage routine cardiovascular screening to aid early detection and prevention of possible abnormalities.
Acknowledgement
The authors wish to thank the Department of Physiology, University of Nigeria, for providing the equipments used for this study.
Conflict of Interest
The authors declare no conflict of interest.
Funding Sources
No external funding was received for this study.
References
- Sokunbi OJ, Okoromah CAN, Ekure EN, Olawale OA, Eke WS. Electrocardiographic pattern of apparently healthy African adolescent athletes in Nigeria. BMC Pediatr2021;21:97. https://doi.org/10.1186/s12887-021-02557-8.
CrossRef - Sharieff GQ, Rao SO. The Pediatric ECG. Emergency Medicine Clinics of North America.2006;24:195-208.
CrossRef - Suresh KP, Chandrasekhar S.Sample size estimation and power analysis for clinical research studies. Journal of Human Reproductive Sciences. 2012; 5(1):7-13.
CrossRef - Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure. Hypertension. (2003); 42:1206-52.
CrossRef - Kligfield P, Gettes LP, Bailey JJ, Childers R, Deal BJ, Hancock EW (2007). Recommendations for the standardization and interpretation of the electrocardiogram: Part I. The electrocardiogram and its technology a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society endorsed by the International Society for Computerized Electrocardiology. Journal of American College of Cardiology. 2007; 49:1109-1127.
- Berson AS., Pipberger, HV. Skin-electrode impedance problems in electrocardiography. American Heart Journal.1968; 76:514–525.
CrossRef - Patterson RP. The electrical characteristics of some commercial ECG electrodes. Journal of Electrocardiology. 1978; 11:23–26.
CrossRef - Olson WH, Schmincke DR, Henley BL. Time and frequency dependence of disposable ECG electrode-skin impedance. Medicine Instrument. 1979; 13:269–272.
- Pipberger HV, Arzbaecher RC, Berson AS, Briller SA, Brody DA, Flowers NC, Geselowitz DB, Lepeschkin E, Oliver GC, Schmitt OH, Spach MS. Recommendations for standardization of leads and of specifications for instruments in electrocardiography and vectorcardiography: report of the Committee on Electrocardiography. Circulation. 1975; 52:11–31.
- Pahlm O, Haisty WK Jr, Edenbrandt L, Wagner NB, Sevilla DC, Selvester RH, Wagner GS Evaluation of changes in standard electrocardiographic QRS waveforms recorded from activity-compatible proximal limb lead positions. American Journal of Cardiology.1992; 69:253–257.
CrossRef - Jacobson J, Garson A Gillette. Premature ventricular contractions in normal children. Pediatric.1978; 92:36–8.
CrossRef - Southall DP, Richards J, Mitchell P (1980). Study of cardiac rhythm in healthy newborn infants. British Heart Journal. 1980; 43:14–20.
CrossRef - Paul T, Marchal C, Garson A Jr. Ventricular couplets in the young: prognosis related to underlying substrate. Am Heart J.1990; 119:577–582.
CrossRef - Dickinson DF, Scott O. Ambulatory electrocardiographic monitoring in 100 healthy teenage boys. Br Heart J.1984; 51:179–183.
CrossRef - Scott O, Williams GJ. Fiddler GI. Results of 24 hour ambulatory monitoring of electrocardiogram in 131 healthy boys aged 10 to 13 years. Br Heart J .1980; 44: 304–308.
CrossRef - Southall DP, Richards J, Mitchell P, Brown DJ, Johnston PG, Shinebourne EA. Study of cardiac rhythm in healthy newborn infants. Br Heart J 1980; 43:14–20.
CrossRef - Nagashima M, Matsushima M, Ogawa A, Ohsuga A, Kaneko T, Yazaki T, Okajima M. Cardiac arrhythmias in healthy children revealed by 24-hour ambulatory ECG monitoring. PediatrCardiol 1987; 8:103–108.
CrossRef - Massin MM, Bourguignont A, Gerard P. Study of cardiac rate and rhythm patterns in ambulatory and hospitalized children. Cardiology. 2005; 103:174–179.
CrossRef - Keany JE, Desai, AD, Schraga, Erik D, ed .Premature Ventricular Contraction. eMedicine. 2017
- Guyton AC, Hall JE. Textbook of medical physiology (11th ed.). Philadelphia: Elsevier Saunders. 2006; 151.
- Kostis JB, Moreyra AE, Amendo MT. The effect of age on heart rate in subjects free of heart disease. Studies by ambulatory electrocardiography and maximal exercise stress test. Circulation. 1982; 65:141 – 5.
CrossRef - Cohen MI. Frequent premature ventricular beats in healthy children: when to ignore and when to treat? CurrOpinCardiol. 2019; 34(1):65-72.
CrossRef - Bertels RA, Harteveld LM, Filippini LH, Clur SA, Blom NA. Left ventricular dysfunction is associated with frequent premature ventricular complexes and asymptomatic ventricular tachycardia in children. Europace. 2017;19(4):617-621.
CrossRef - Dick M, O’Connor B, Serwer G, LeRoy S, Armstrong B.Use of radiofrequency energy to ablate accessory connections in children. Circulation.1991; 84(23):18-24.
CrossRef - LeRoy S, Dick M. Supraventricular tachycardia. In Zeigler VL & Gillette P, eds. Practical management of pediatric cardiac arrhythmias. Armonk, New York: Futura Publishing Co.2001. 53-109.
- Weindling SN, Saul JP, Walsh EP. Efficacy and risks of medical therapy for supraventricular tachycardia in neonates and infants. American Heart Journal. 1996; 131(1):66-72.
CrossRef - Gillette PC, Garson A. Electrophysiologic and pharmacologic characteristics of automatic ectopic atrial tachycardia. Circulation.1977;56:571–575.
CrossRef - Keane JF, Plauth WH, Nadas AS. Chronic ectopic tachycardia of infancy and childhood. Am Heart J., 1972;84:748–757.
CrossRef - Koike K, Hesslein PS, Finlay CD, Williams WG, Izukawa T, Freedom RM. Atrial automatic tachycardia in children. Am J Cardiol., 1988; 61:1127–1130.
CrossRef - Chiladakis JA, Vassilikos VP, Maounis TN, Cokkinos DV, Manolis AS. Successful radiofrequency catheter ablation of automatic atrial tachycardia with regression of the cardiomyopathy picture. Pacing Clin Electrophysiol. 1997; 20:953–959.
CrossRef - Gillette PC, Smith RT, Garson A, Mullins CE, Gutgesell HP, Goh TH, Cooley DA, McNamara DG. Chronic supraventricular tachycardia. A curable cause of congestive cardiomyopathy. JAMA. 1985;253:391–392.
CrossRef - Kugler JD, Baisch SD, Cheatham JP, Latson LA, Pinsky WW, Norberg W, Hofschire PJ. Improvement of left ventricular dysfunction after control of persistent tachycardia.JPediatr. 1984;105:543–548.
CrossRef - Gillette PC, Smith RT, Garson Jr A, Mullins CE, Gutgesell HP, Goh TH, et al. Chronic supraventricular tachycardia. Acurable cause of congestive cardiomyopathy. JAMA. 1985; 253(3):391-392.
CrossRef - Fishberger SB, Colan SD, Saul JP, Mayer Jr JE, Walsh EP. Myocardial mechanics beforeand after ablation of chronic tachycardia. Pacing Clin Electrophysiology. 1996; 19(1):42-49.
CrossRef - Houmsse M, Tyler J, Kalbfleisch S. Supraventricular tachycardia causing heart failure. CurrOpinCardiol. 2011;26(3):261-269.
CrossRef - Bonney WJ, Shah MJ. Incessant SVT in children: Ectopic atrial tachycardia and permanent junctional reciprocating tachycardia. Progress in Pediatric Cardiol. 2013; 35(1):33-40.
CrossRef - Salerno J, Seslar S, Chun T, Vafaeezadeh M, Parrish A, Permut L. Predictors of ECMO support in infants with tachycardia-induced cardiomyopathy. PediatrCardiol. 2011; 32(6):754-758.
CrossRef - Walsh EP. Automatic atrial and junctional tachycardias. In: Walsh EP, Saul JP, Triedman JK, editors. Cardiac arrhythmias in children and young adults with congenital heart disease. Philadelphia: Lippincott Williams & Wilkins. 2001: 11-123.
- Martin CA, Lambiase PD. Pathophysiology, diagnosis and treatment of tachycardiomyopathy. Heart. 2017; 103(19):1543-1552.
CrossRef - Toyohara K, Fukuhara H, Yoshimoto J, Ozaki N, Nakamura Y. Electrophysiologicstudies and radiofrequency catheter ablation of ectopic atrial tachycardia in children. PediatrCardiol. 2011; 32(1):40-46.
CrossRef - Mehta AV, Sanchez GR, Sacks EJ, Casta A, Dunn JM, Donner RM. Ectopic automaticatrial tachycardia in children: Clinical characteristics, management and follow-up. J Am Coll Cardiol. 1988; 11(2):379-385.
CrossRef - PremSekar R. Epidemiology of Arrhythmias in Children. Indian Prem pacing Electrophysiology journal. 2008; 8: S8–S13.
- Lewalter T, Pürerfellner H, Ungar A, Rieger G, Mangoni L, Duru F., INSIGHT XT study investigators. “First-degree AV block-a benign entity?” Insertable cardiac monitor in patients with 1st-degree AV block reveals presence or progression to higher grade block or bradycardia requiring pacemaker implant. J Interv Card Electrophysiol. 2018;52(3):303-306. [PubMed] CrossRef
- Lee S, Singla M. An Unrecognized Rash Progressing to Lyme Carditis: Important Features and Recommendations Regarding Lyme Disease. Am J Ther. 2016 Mar-Apr; 23(2):e566-9.
CrossRef - Rojas LZ, Glisic M, Pletsch-Borba L, Echeverría LE, Bramer WM, Bano A, Stringa N, Zaciragic A, Kraja B, Asllanaj E, Chowdhury R, Morillo CA, Rueda-Ochoa OL, Franco OH, Muka T. Electrocardiographic abnormalities in Chagas disease in the general population: A systematic review and meta-analysis. PLoSNegl Trop Dis. 2018; 12(6):e0006567.
CrossRef - Mantovani A, Rigolon R, Pichiri I, Morani G, Bonapace S, Dugo C, Zoppini G, Bonora E, Targher G. Relation of elevated serum uric acid levels to first-degree heart block and other cardiac conduction defects in hospitalized patients with type 2 diabetes. J. Diabetes Complicat. 2017; 31(12):1691-1697.
CrossRef - Steve G, Karen M. Pediatric Electrocardiography. British Medical Journal series. 2002;324; 1382-1385.
CrossRef - Cheng S, Keyes MJ, Larson MG, McCabe EL, Newton-Cheh C, Levy D, Benjamin EJ, Vasan RS, Wang TJ. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA. 2009; 24; 301(24):2571-2577.
CrossRef - Kelly RE, Carter R, Larry W, Kathleen, RM. Just sinus bradycardia or something more serious? Case Reports in Pediatrics.2013: 1-5.
CrossRef - Yamakawa Y, Ishikawa T, Uchino K, et al. Prevalence of right bundle-branch block and right precordial ST-segment elevation (Brugada-type electrocardiogram) in Japanese children. Circ J. 2004; 68:275–9.
CrossRef - Marc DL . Paediatric Cardiology: Paediatric Electrophysiology and Pacing.Journal of the American College of Cardiology. 2009; 54:4-6.
- Macfalane PW, MeLaughlin SC, Devine B, Yang TF. Effect of age sex and race on ECG interval measurements. Journal of Electrocardiology.1994;27:14-19
CrossRef - Xie ZW, Wang C, LiMX . Electrocardiographic QRS waves of healthy Chinese population with different ages and sexes. Hunan Yi Ke Da XueXueBao.2000;25:58-62.
- Xie Z, Wang C, Li MX. Electrocardiographic T-wave amplitude of normal population and its correlation with age sex and race. Hunan Yi Ke Da XueXueBao.1999;24:335-340.
- Walker AR, Walker BF. The bearing of race sex age and nutritional state on the precordial electrocardiograms of young South African Bantu and Caucasian subjects. American Heart Journal.1969;77:441-459.
CrossRef - Paecha M, Anhalta RA, Gebauera F, Wagnera M, Vogelb T. Kirstenc M, Weidenbacha W, Kieddb I, Dahnerta A, Kornerb . New normal limits for pediatric ECG in childhood obesity? Influence of childhood obesity on the ECG. Progress in Pediatric Cardiology. 2018; 48: 119-123.
CrossRef - Hiss RG, Lamb LE. Electrocardiographic findings in 122, 043 individuals. Circulation.1962 25:947-961.
CrossRef - Jones J, Srodulski ZM, RomisherS . The aging electrocardiogram. American Journal Emergency Medicine. 1990; 80:240 – 245.
CrossRef

This work is licensed under a Creative Commons Attribution 4.0 International License.





