Manuscript accepted on : April 22, 2011
Published online on: 28-06-2011
Oral Manifestation in Tuberculosis Disease: A Case Report
Shivayogi Charanthimath1 and Raghvendra Byakodi2
1Department of Oral Medicine & Radiology, KLE's Vishwanath Katti Institute of Dental Sciences Belgaum India.
2Departement of Oral and Maxillofacial Surgery, Bharathi Vidyapeeth University Dental College and Hospital. Sangli India.
ABSTRACT: Tuberculosis is one of the major causes of ill health and death world wide. Since the introduction of effective chemotherapy, tuberculosis lesions of the oral cavity are rare. Most of the cases are secondary to pulmonary disease and the primary form is uncommon. In this paper, we present a case of oral tuberculosis , involving the soft palate in a 32yr old male patient and differential diagnosis is discussed.
KEYWORDS: tuberculosis; palate
Download this article as:| Copy the following to cite this article: Charanthimath S, Byakodi R. Oral Manifestation in Tuberculosis Disease: A Case Report. Biosci Biotech Res Asia 2011;8(1) |
| Copy the following to cite this URL: Charanthimath S, Byakodi R. Oral Manifestation in Tuberculosis Disease: A Case Report. Biosci Biotech Res Asia 2011;8(1). Available from: https://www.biotech-asia.org/?p=9370 |
Introduction
Tuberculosis is a chronic granulomatous disease commonly presenting as pulmonary tuberculosis1.According to the World Health Organization; tuberculosis is responsible for death of approximately 2 million people each year. Extra pulmonary involvement in tuberculosis is less frequent contributing to 10-15% of cases. Involvement of oral cavity is rare accounting for 0.2-0.5 % of cases. Oral tuberculosis lesions may be either primary or secondary, although there are also reports of atypical cases in the literature.1
Tongue, gingival and palate are the most common sites to be involved in oral tuberculosis. The clinical presentation of tuberculosis may take many forms like ulcer, nodule, granuloma and fissure however, with the decline in numbers, tuberculosis lesion of oral cavity have become so rare that they are frequently overlooked in the differential diagnosis of oral lesion.2
The aim of this paper was to report a case of oral tuberculosis involving palate observed in Department of Oral Medicine Diagnosis and Radiology at Bharati Vidyapeeth University Dental College Sangli.
Case report
A 33 yr old male patient (FIGURE 1 Patient profile) reported to the Department of Oral Medicine Diagnosis and Radiology with chief compliant of painful ulcer in oral cavity since 2 months and had remained unhealed .
 |
Figure 1 Patient profile.
|
On questioning patient revealed that he was on medication for tuberculosis since 6 months, and he was operated for ulcer in gastrointestinal tract for which endoscopic report of Chrons disease was given. General physical examination showed , well developed, undernourished man . On palpation submandibular lymp nodes were enlarged, non tender and freely movable with no evidence of matting and he was also gutka chewer since 5 years.
Intra oral examination revealed a reddish nodule measuring approximately 3.5mm in diameter on right side of soft palate. It was indurated and bound to underlying structures on palpation as shown in (Figure2).Blanching was observed on palate and oral mucosa bilaterally. A erosion measuring around 2×2 mm in diameter was seen on soft palate at left side as shown in (Figure 2) and similar lesion was observed in right buccal mucosa as shown in (Figure3 ).
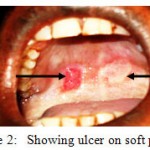 |
Figure 2: Showing ulcer on soft palate.
|
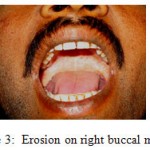 |
Figure 3: Erosion on right buccal mucous.
|
On palpation vertical fibrous bands felt on right and left buccal mucosa extending upto retromolar pad and circum oral bands felt on labial mucosa, tongue movement reduced .
Based on history and clinical features a provisional diagnosis of tubercular ulcer on soft palate and oral submucous fibrosis was given.
Mycotic infection, Chrons disease, and malignancy were considered in differential diagnosis
Further patient underwent physical examination and total blood investigation, including ELISA test for HIV status which reported normal and negative HIV status. .
Since the patient was on antitubercular drugs (AKT 2.) Rifampicin 450mg+isoniazid 300mg.An increase of dosage was recommended to the patient under physician guidance instead of surgical intervention.
Treatment Plan: 1. Tab Rifampicin 450mg, Tab Isoniazid 300mg, Tab Etambutol 800mg for 2 months (AKT-3)
2 Kenacort 0.1% – Topical application buccal mucosa- 7 days
Mouth wash – Chlorhexidine 0.12%
Prognosis: The patient was recalled for follow-up after 1 weak which resulted in complete remission of lesion on palate as shown in( Figure no 4) and healed erosion on right buccal mucousa.(Figure 5).
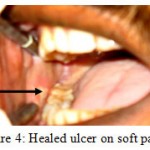 |
Figure 4: Healed ulcer on soft palate.
|
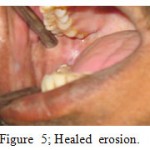 |
Figure 5: Healed erosion.
|
Discussion
Tuberculosis is a chronic infectious granulomatous disease caused in human beings by M. tuberculosis and less frequently by M. bovis. The oral lesions of the disease although not common, occur in various forms. They may appear as ulcers, nodules, fissures, tuberculomas or granuloma and are usually caused by pulmonary diseases, whereas primary involment is considered to be rare.2
The most frequent lesion is the ulcer which is characterized by undermined edges with minimal induration occasionally small tuberculosis nodules are around the periphery. The base of the ulcer may be granular or covered with a pseudo- membrane. The tongue is one of the organs most commonly affected. Other oral sites are the floor of the mouth, soft palate, gingival, lips, and hard palate. Secondary tuberculosis of the mouth may be seen in all age groups; however middle aged and older persons are more likely to have oral manifestation of the disease, which is almost always painful.3, 4 and 5
Rarely the oral mucosa has been reported to be the site of the first invasion by the tubercle bacilli. Primary involment is more common in children and adolescents than adults. It usually presents as a single painless indolent ulcer, commonly on the gingival, which progressively extends from the gingival margin to the depths of the adjacent vestibule and is often associated with enlarged cervical lymph nodes.6
Clinical diagnosis can be difficult because tuberculosis can mimic a variety of other conditions, including malignancy, traumatic and apthous ulcer, syphilis, sarcoidosis Wagener’s granulomatosis and deep fungal infection such as paracoccidiomycosis and histoplasmosis1
For confirmation and differential diagnosis, Mantoux reaction , biopsy for histological examination, acid fast stains and culture should be obtained .Positive tuberculin skin test just indicates previous exposure to the M tuberculosis . Although presumptive diagnosis of tuberculosis can be based on histopathological examination and identification of the bacilli in tissue using special stains, because of the relative scarcity of the bacilli within tissue mycobacterium can be demonstrated by means of special stains only in 27-60% of cases. Radiographic evidence of tuberculosis must also be sought.7
In our case as the ulcer was seen on, soft palate with undermined edges, non healing, since 2 months a clinical diagnosis of tuberculosis ulcer was given and differential diagnosis of malignancy, fungal infection, Chrons disease was included.
As our patient was known case of tuberculosis, with confirmed biopsy report and smear test was not advised. The treatment plan included increase of dosage of rifampicin, isoniazid, and Ethambutol which are potent anti-tubercular drugs. As our patient had OSMF kenacort topical application was advised to reduce burning sensation, and intralesion injections of corticosteroid was contraindicated as patient immunity was suppressed. An attempt of healing the ulcer on medicine has been done in our case. A, follow up for 1 month was done, with good prognosis and healed ulcer on palate, and buccal mucousa. In conclusion , tuberculous ulcer should be considered while diagnosing non healing ulcer in the oral cavity and they can be effectively treated with anti tuberculosis regimen. Since our patient was already on a treatment regimen, we increased the dose which led to rapid healing of the ulcer. So any lesion on soft palate should be suspected for tuberculosis, and should be treated with antitubercular drugs by increasing the regime dosage which have good prognosis as seen in our case.
The identification of a tuberculosis lesion in any location in the mouth is an unusual
Finding and its discovery is usually indicative of underlying pulmonary disease. . This helps not only in complete diagnosis but also in better patient management. All such cases should promptly receive anti- tuberculosis therapy because oral lesions pose a potential infectious hazard to dental personnel.
References
- FA Ito, CR de Andrade, PA Vargas, J Jorge, Ma Lopes. Primary tuberculosis of the oral cavity Case report. Oral Diseases. (2005) 11, 50-53
- Praveen B.N, Sumati,.Kori, Balagi Rao . Primary Oral Tuberculosis-A Case Report IAOMR 2007, 19; 04,529-532
- Ioannis Dimtrakopoulos ,Lambros Zouloumis, Nicolaos Lazaridis. Primary tuberculosis of the oral cavity. Oral Surg Oral Med Oral Pathol 1991; 72:712-5
- Haddad NM, Zaytoun GM, Hadi U Tuberculosis of the soft palate: an unusual presentation of oral tuberculosis. Otolaryngol Head and Neck Surg 1987:97; 91-9
- Hashimoto y, Tanioka H. Primary tuberculosis of the tongue. Report of cas J Oral Maxillofac surg 1989; 47: 744-6.
- Nolte WA. Oral microbiology. St Louis; CV Mosby, 1982:433-40
- D.P. Von Arx, A Husain. Oral Tuberculosis .British Dental Journal 2001 Vol. 190, no 8 :420-422.

This work is licensed under a Creative Commons Attribution 4.0 International License.





